Case 4
Authors: Melissa Argraves, MD & Pamela Weiss, MD, MSCE
Case History
A 13-year-old male presents with left hip and right-sided low back pain.
He reports:
- 1 year of left hip pain, worse at the end of the day
- Over last 6 months, he has also developed right lower back/buttock pain
- 15 minutes of morning stiffness in back and legs
- Right buttock pain is worse with prolonged sitting
Review of Systems: No diarrhea, no bloody stool, no rashes, no fevers, no weight loss, no joint swelling
Past Medical History: Non-contributory
Family History: Mother- juvenile idiopathic arthritis (subtype unknown), no inflammatory bowel disease, no psoriasis, no other autoimmune disease
Immunizations: Up to date
Allergies: No known drug allergies
Medications: Naproxen 375 mg twice daily (10 mg/kg twice daily)
Physical Exam:
General: Normal vital signs, Weight 37.5 kg, Well appearing
HEENT: Normal
Chest/Lungs: Normal
Abdomen: Normal
Skin: No rashes. No nail pits.
Joints: Pain at the right buttock with external rotation and abduction of the left hip, no peripheral arthritis, hip ROM normal
Entheses: Right sacroiliac tenderness, left greater trochanter tenderness
Question 1
What is the best study to evaluate for sacroiliitis in children?
- X-ray pelvis
- CT pelvis
- Non-contrast MRI pelvis
- LS Spine MRI with contrast
C. Non-contrast MRI pelvis
MRI is the best imaging modality to evaluate for pediatric sacroiliitis. X-rays are not sensitive and MOST children with sacroiliitis do not have x-ray evidence of disease. CT scan is also not an ideal study and exposes children to unnecessary radiation. MRI of the pelvis without contrast is equivalent to a contrast study if STIR or T2 fat saturated & T1 sequences are obtained. Avoidance of contrast is both safer for the patient and cheaper. Lumbosacral imaging may or may not appropriately visualize the sacroiliac joint depending on the protocol used and as noted above, contrast is unnecessary.
Work Up
- CBC, CMP normal
- CRP 2.1 mg/dL
- ESR 37 mm/hr
- HLA-B27 positive
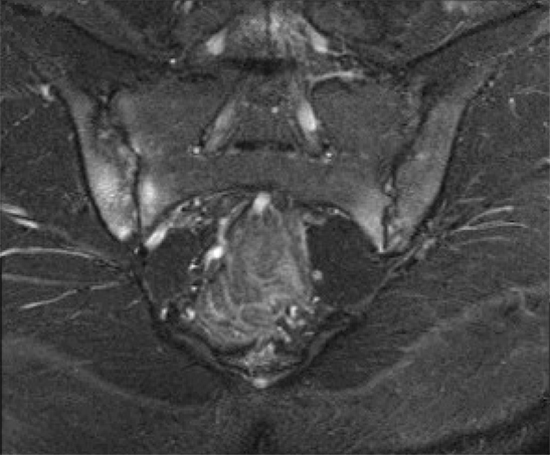
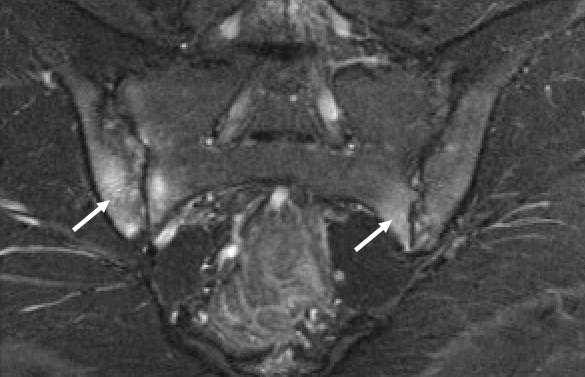
- MRI Pelvis – See figure 1
Question 2
Which imaging finding is required for radiologic diagnosis of pediatric sacroiliitis on MRI imaging?
- Surrounding bone marrow edema
- Fluid within the sacroiliac joint space
- Bony erosions
- Synovial enhancement
A. Surrounding bone marrow edema
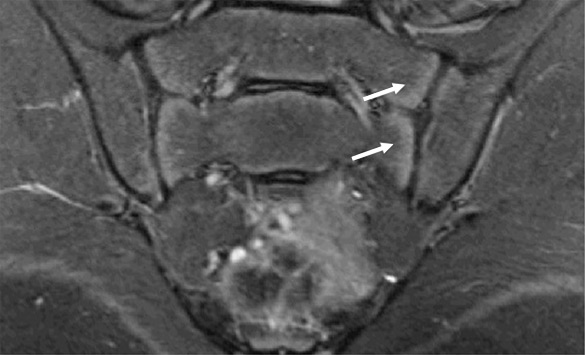
Our patient (figure 1) had clear evidence of sacroiliitis with bone marrow edema (arrows). Healthy pre-pubertal and some peri-pubertal youth have metaphyseal equivalent subchondral signal that is symmetric, follows the contour of the bone and often also extends within the cartilage of the sacral bodies (figure 2 arrows) that should not be mistaken for inflammation. Erosions are evidence of more chronic disease and do not need to be seen to make the diagnosis of sacroiliitis.
Question 3
What is the best choice of therapy for this patient?
- TNF inhibitor
- Switch to a different NSAID
- Methotrexate
- Oral corticosteroids
A. TNF inhibitor
This patient is symptomatic despite appropriate dose of NSAIDs and has bilateral sacroiliitis with bone marrow edema and erosions. Medication is usually dosed by weight in children, and appropriate dosage of naproxen for treatment of arthritis related pain and inflammation is 10 mg/kg twice daily. In cases like this the ACR/AF JIA guidelines recommend TNF inhibition. While NSAIDs, are preferred over no treatment, TNF inhibition is preferred. TNF inhibition is also preferred over methotrexate monotherapy.
Case Continued: Question 4
The patient’s 10-year-old brother is diagnosed with enthesitis-related arthritis two years later after presenting to rheumatology with right knee and ankle swelling as well as tenderness over the Achilles insertions bilaterally. He is also HLA-B27 +.
What additional finding is most likely to be predictive of sacroiliitis?
- Back pain
- Elevated CRP
- SI tenderness
- Elevated ESR
B. Elevated CRP
“Silent” sacroiliac disease can occur in children with enthesitis related arthritis meaning that the patients do not have symptoms or exam findings. Risk factors for silent disease include hip arthritis, HLA-B27 positivity and elevation of CRP. Silent sacroiliac disease (both subchondral edema and evidence of damage) can be present at time of diagnosis in up to 20% of youth.
Pediatric Case 4 Feedback
"*" indicates required fields
References
- Weiss PF, Xiao R, Biko DM, Chauvin NA. Assessment of Sacroiliitis at Diagnosis of Juvenile Spondyloarthritis by Radiography, Magnetic Resonance Imaging, and Clinical Examination. Arthritis Care Res (Hoboken). 2016 Feb;68(2):187-94. doi: 10.1002/acr.22665. PMID: 26212574; PMCID: PMC4720597.
- Ringold S, Angeles-Han ST, Beukelman T et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Care Res (Hoboken). 2019 Jun;71(6):717-734. doi: 10.1002/acr.23870. Epub 2019 Apr 25.
- Weiss PF, Xiao R, Brandon TG, et al. Radiographs in screening for sacroiliitis in children: what is the value? Arthritis Res Ther 2018;20(1):141.
- Jaremko JL, Liu L, Winn NJ, et al. Diagnostic utility of magnetic resonance imaging and radiography in juvenile spondyloarthritis: evaluation of the sacroiliac joints in controls and affected subjects. J Rheumatol 2014;41(5):963e70.
- Weiss, Pamela F., and Nancy A. Chauvin. “Imaging in the diagnosis and management of axial spondyloarthritis in children.” Best Practice & Research Clinical Rheumatology (2020): 101596.
- Stoll, Matthew L., et al. “Spondyloarthritis in a pediatric population: risk factors for sacroiliitis.” The Journal of rheumatology 37.11 (2010): 2402-2408.