Case 3
Authors: Olivia Kwan, MD, Melissa Oliver, MD MS
A 13-year-old male presents with pain in his neck, upper back, knees and hips for the past 5 years.
- His pain is daily, constant and described as achy.
- It is worse with activities. He has quit all sports except for swimming due to the pain. His pain limits his daily activities and he needs assistance with getting up and sitting down.
- He has morning stiffness for a few hours.
- He had some relief from ibuprofen or naproxen when taken as needed.
Review of systems: Positive for poor linear growth over the last five years. Negative for fevers, night sweats, weight loss, rash, GI symptoms, oral ulcers or eye redness and eye pain.
Family History: Mother with Crohn’s disease on infliximab.
Clinical Exam:
Normal vital signs
General, head and neck, cardiovascular, respiratory, skin and neurologic systems: Normal.
Musculoskeletal:
- Bilateral shoulder exam noted mild limitation of range of motion and pain that was worse in the left shoulder
- Bilateral hip exam noted external rotation limitation to 5 degrees with pain
- Spine- Cervical: pain on range of motion. Extension 60 degrees and lateral rotation to 75 degrees bilaterally. Lumbar: tenderness to palpation
- FABER- noted to have ipsilateral groin pain bilaterally
- Modified Schober: Limited, 12.5cm
- Sacroiliac joints– nontender bilaterally
- Unable to lie flat on back secondary to pain
- Gait- antalgic
- Otherwise a complete joint and entheseal count was performed and there were no other signs of swelling, tenderness, or limitation in range of motion.
Lab Findings
Complete blood count normal
Comprehensive metabolic panel normal
ESR 51 mm/hr (ref range: 0-15 mm/hr)
CRP 3.63 mg/dL (ref range: <0.5 mg/dl)
ANA 1:80
Anti-dsDNA negative
HLAB27 negative
LDH normal
Uric Acid normal
Imaging
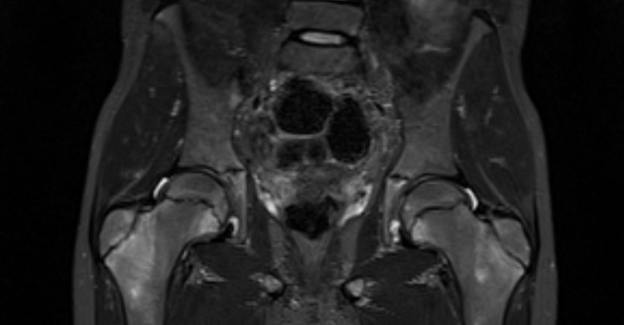
MRI of the pelvis without contrast showed normal SI joints (not shown) and bone marrow edema throughout the bilateral femoral metaphysis and greater trochanter (shown)
Based on this information what is the most likely diagnosis?
- Infectious osteomyelitis
- Chronic nonbacterial osteomyelitis
- Intraosseous lymphoma
- Enthesitis related arthritis
B. Chronic nonbacterial osteomyelitis
Chronic nonbacterial osteomyelitis (CNO) is an autoinflammatory bone disease of unknown cause (1). While some patients develop unifocal and time-limited disease, most experience chronically active or recurrent disease affecting multiple bones, known as chronic recurrent multifocal osteomyelitis (CRMO). CNO commonly presents with bone pain, normal or mildly elevated inflammatory markers and imaging findings of hyperintense signal of bone on MRI and lytic and/or sclerotic lesions on X-rays later in the disease. It is generally a diagnosis of exclusion. The most common mimickers are infectious osteomyelitis and malignancy, such as intraosseous lymphoma. It is important to rule those out before making a diagnosis. In some cases, bone biopsies may need to be performed to aid in ruling out mimicker disease. In our case, since his symptoms have been present for 5 years, there were no fevers, there was a symmetric appearance on MRI and his complete blood count was normal, infectious osteomyelitis is less likely. Additionally, given the duration, normal complete blood count, LDH, uric acid and lack of constitutional symptoms (fevers, night sweats, or weight loss), malignancy is also less likely. Juvenile ankylosing spondylitis is also less likely given the normal SI joints and bone marrow edema at the femoral metaphysis findings, which is a characteristic radiographic finding in CNO patients.
- Zhao Y, Ferguson PJ. Chronic nonbacterial osteomyelitis and chronic recurrent multifocal osteomyelitis in children. Pediatric Clinics. 2018 Aug 1;65(4):783-800.
What further imaging would you do to help with the diagnosis of CRMO?
- MRI of the lumbar spine
- Bone Scan
- CT spine
- Whole body MRI
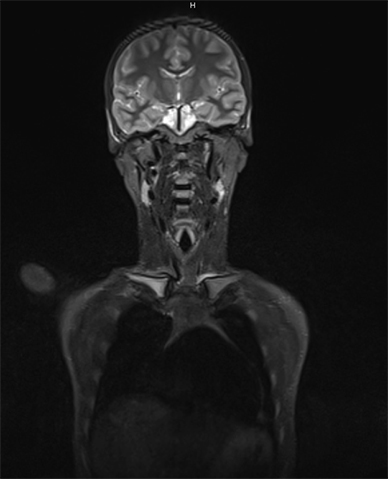
D. Whole body MRI
As patients may initially present with focal bone pain, it is not uncommon for dedicated imaging of that area to be obtained. However, once CRMO is suspected, a whole-body MRI is the preferred imaging modality to assess for asymptomatic lesions, establish a disease baseline and follow for response to treatment (1, 2).
- Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS, Lee TC, Fox E, Amarilyo G, Stern SM, Dvergsten JA. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis care & research. 2018 Aug;70(8):1228-37.
- Schnabel A, Range U, Hahn G, Berner R, Hedrich CM. Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44(7):1058–65.
Treatment
What is the most appropriate initial treatment for suspected CRMO?
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Tumor necrosis factor inhibitors (TNFi)
- Bisphosphonates
- Methotrexate
- Sulfasalazine
A. Non-steroidal anti-inflammatory drugs (NSAIDs)
Initial treatment options for CRMO/CNO includes NSAIDs. About half of patients will have complete clinical remission on NSAID therapy, but many will only experience a partial response or continue to have flares.
Other treatment options include DMARDs such as methotrexate and sulfasalazine, TNFi such as adalimumab, etanercept, and infliximab, and bisphosphonates like pamidronate and zoledronic acid. For management of an acute flare, NSAIDs and low-medium dose glucocorticoids have been used (1, 2).
- Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS, Lee TC, Fox E, Amarilyo G, Stern SM, Dvergsten JA. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis care & research. 2018 Aug;70(8):1228-37.
- Schnabel A, Range U, Hahn G, Berner R, Hedrich CM. Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44(7):1058–65.
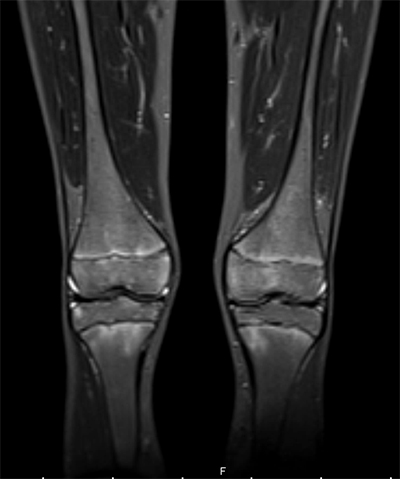
The whole-body MRI shows symmetric bone marrow edema within the pelvis, metaphyses & epiphyses of bilateral femora (shown), tibia, proximal humerii and asymmetric bone marrow edema in the medial clavicle (shown), right acromial process, L4 spine superior endplate, left ischium and left iliac crest.
Would this new information from the whole-body MRI change your treatment plan?
- yes
- no
A. yes
Spinal lesions in CNO are considered high risk lesions and therefore should be treated more aggressively, generally with bisphosphonates. These patients should not be started on NSAIDs alone due to the risk of developing a vertebral fracture. The extensive multifocal nature of his disease presentation may also warrant additional immunosuppression with DMARDs and/or TNFi (1).
- Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS, Lee TC, Fox E, Amarilyo G, Stern SM, Dvergsten JA. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis care & research. 2018 Aug;70(8):1228-37.
Follow Up
You treat your patient and he is doing well on therapy combination of NSAIDs, Methotrexate and bisphosphonate, but one year later he returns for follow up with a new rash.
What is going on now with your patient?
- Medication side effect
- New onset psoriasis
- Palmoplantar pustulosis
- Contact dermatitis
C. Palmoplantar pustulosis
This is palmoplantar pustulosis (PPP). About 10-30% of patients can develop skin manifestations.There is also a related syndrome called Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis (SAPHO) that primarily presents in adults, but can also manifest in children and adolescents. SAPHO may be part of CNO’s disease spectrum or its presentation in a different age group. The degree of skin involvement and location of osteitis may help distinguish these entities. The peripheral skeleton is more often affected in CNO, whereas, in SAPHO, the axial skeleton and costosternoclavicular region are more often involved. The most classic skin lesions seen in persons with SAPHO include palmoplantar pustulosis (PPP) and acne. Skin manifestations do not always occur with the musculoskeletal symptoms and can appear many years later after the onset of bone manifestations (1-4).
- Skrabl-Baumgartner A, Singer P, Greimel T, Gorkiewicz G, Hermann J. Chronic non-bacterial osteomyelitis: a comparative study between children and adults. Pediatric Rheumatology. 2019 Dec;17(1):49.
- Letts M, Davidson D, Birdi N, Joseph M. The SAPHO syndrome in children: a rare cause of hyperostosis and osteitis. Journal of Pediatric Orthopaedics. 1999 May 1;19(3):297-300.
- Roderick MR, Sen ES, Ramanan AV. Chronic recurrent multifocal osteomyelitis in children and adults: current understanding and areas for development. Rheumatology. 2018 Jan 1;57(1):41-8.
- Rohekar G, Inman RD. Conundrums in nosology: synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome and spondylarthritis. Arthritis Rheum. 2006;55(4):665–9.
Pediatric Case 3 Feedback
"*" indicates required fields
