Case 2
Author: Matthew Stoll MD, PhD
Patient is an 11-year-old male presenting with low back pain and stiffness ongoing for several months. Symptoms worse in the morning, improved with stretching and activity. Has taken ibuprofen 400 mg twice daily for two months with transient symptomatic relief. No other areas of joint pain.
Past medical history: Negative
Family history: Negative for arthritis, inflammatory bowel disease (IBD), or psoriasis
Social history: Lives with parents. Attends school in the 5th grade.
Review of systems: Negative
On exam, there is no peripheral arthritis. The patient had tenderness over his sacroiliac joints (SIJ) bilaterally, as well as positive FABER and SIJ distraction maneuvers.
Labs showed WBC 8.6, Hb 9.3, Plt 459.
ESR 58 mm/hr, CRP 3.6 mg/dL
Normal comprehensive metabolic panel
Negative HLA-B27
X-ray of SIJ was normal / negative. MRI of SI joints showed bone marrow edema in the sacrum and to a lesser extent the left ileum (Figure 1.)

Which of the following therapies is most appropriate to recommend for this patient?
- Prednisone taper over six months
- Methotrexate
- Sulfasalazine
- TNF inhibitor
4. TNF inhibitor
His symptoms and imaging findings are most consistent with sacroiliitis secondary to enthesitis related arthritis. Although prednisone may provide symptomatic relief and can be considered as bridge therapy, long-term use of corticosteroids to manage JIA is inappropriate. Traditional disease modifying anti-rheumatic drugs such as methotrexate and sulfasalazine are not of benefit in the management of axial spondyloarthritis, so treatment recommendations in such patients are to proceed directly to TNF inhibition after failure of non-steroidal anti-inflammatory drugs [1].
He was initially started on adalimumab but did not tolerate the injections due to local site reaction, so he was switched to etanercept. His symptoms improved quickly, and his laboratory findings normalized.
However, 2 – 3 years later, he developed abdominal pain and bloody diarrhea lasting several months. There was no preceding travel, illness, or antibiotic use. On exam, he had generalized abdominal tenderness.
Labs: WBC 10.8, Hb 10.5, Plt 535
ESR 59, CRP 9.9 mg / dL
Fecal calprotectin level was 5950 μg/g (negative < 50; borderline 50 – 120.)
Which of the following is the next best step?
- Referral to GI for ileocolonoscopy
- Cognitive behavioral therapy for irritable bowel syndrome
- Antibiotic therapy for suspected Clostridioides (formerly Clostridium) difficile infection
- Increase the etanercept dose due to enthesitis related arthritis (ERA) flare.
1. Referral to GI for ileocolonoscopy
About 50 – 60% of patients with spondyloarthritis have sub-clinical intestinal inflammation, and about 5 – 10% develop frank inflammatory bowel disease (IBD) [2, 3] . Conversely, arthritis is a major extra-intestinal manifestation of IBD, present in up to 25% of such patien ts [ 4] . Thus, this patient’s risk of IBD is substantially higher than that of the general population. Furthermore, he has objective evidence of systemic and intestinal inflammation. He does not have any risk factors for C. difficile infection. Increasing the etanercept dose is unlikely to be of benefit, as it is not an effective treatment for IBD [5].
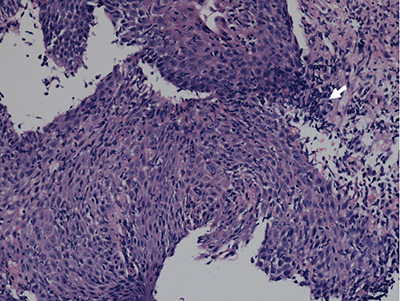
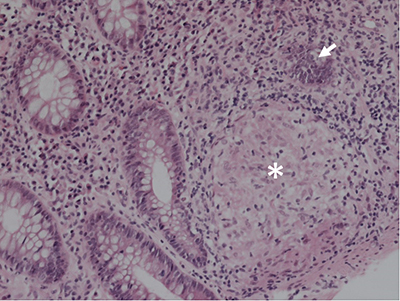
The patient was referred to Gastroenterology and underwent ileocolonoscopy, which demonstrated diffuse colitis and ileitis, with biopsies demonstrating neutrophilic crypt abscesses and granulomas (Figures 2 and 3.) He was diagnosed with Crohn’s Disease and switched from etanercept back to adalimumab, with improvement of his symptoms and normalization of his labs.
Pediatric Case 2 Feedback
"*" indicates required fields
References
- Ringold, S., et al., 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Rheumatol, 2019. 71(6): p. 846-863.
- Fragoulis, G.E., et al., Inflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment. World J Gastroenterol, 2019. 25(18): p. 2162-2176.
- Mielants, H., et al., Gut inflammation in the spondyloarthropathies: clinical, radiologic, biologic and genetic features in relation to the type of histology. A prospective study. J Rheumatol, 1991. 18(10): p. 1542-51.
- Levine, J.S. and R. Burakoff, Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y), 2011. 7(4): p. 235-41.
- Sandborn, W.J., et al., Etanercept for active Crohn’s disease: a randomized, double-blind, placebo-controlled trial. Gastroenterology, 2001. 121(5): p. 1088-94.